| Original Article |
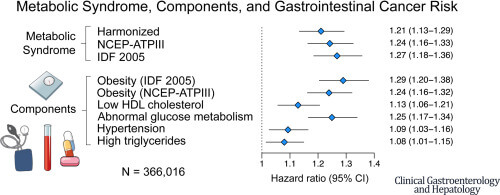
Question: What are the associations between metabolic syndrome (MetS) and gastrointestinal cancer risk?
Design/Method: A prospective cohort study was done based on the UK bio-bank data from 2006 to 2013. MetS status was determined by 3 different definitions at baseline at a repeat assessment after a median of 4.3 years of follow-up. Multivariable hazard ratios and 95% confidence intervals for cancer outcomes were estimated using Cox proportional hazards models. Analyses stratified by polygenic risk score were conducted for colorectal and pancreatic cancers
Setting: The United Kingdom
Patient/Study community: Patients with gastrointestinal cancer and comprehensive serum biomarker and genotype data
Results: MetS is associated with increased risks of colorectal cancer, colon cancer, rectal cancer, hepatocellular carcinoma, pancreatic cancer in women, and esophageal adenocarcinoma in men. Associations for colorectal cancer and pancreatic cancer do not differ by polygenic risk score strata (P-heterogeneity 0.70 and 0.69, respectively)
Commentary:
| Long-term MetS is strongly linked to an increased risk of gastrointestinal cancer in general. The strongest influences on these correlations are abnormal glucose metabolism and obesity. Maintaining excellent metabolic health minimizes the incidence of gastrointestinal malignancies and can help in the development of prophylactic measures since MetS status is unlikely to alter over the long run |
Citation: Joseph A. Rothwell, Mazda Jenab, Mojgan Karimi, et all. Metabolic Syndrome and Risk of Gastrointestinal Cancers: An Investigation Using Large-scale Molecular Data. Clinical Gastroenterology and Hepatology. 2022; 20(6):1338–1352
DOI: 10.1016/j.cgh.2021.10.016
https://pubmed.ncbi.nlm.nih.gov/34687971/
Topics: Cancer Genetic Risk, Cancer Prevention, Gastrointestinal Neoplasms, Molecular Epidemiology
(NCEP-ATPIII: National Cholesterol Education Program – Adult Treatment Panel IIIIDF 2005: International Diabetes Federation)