| Guideline |
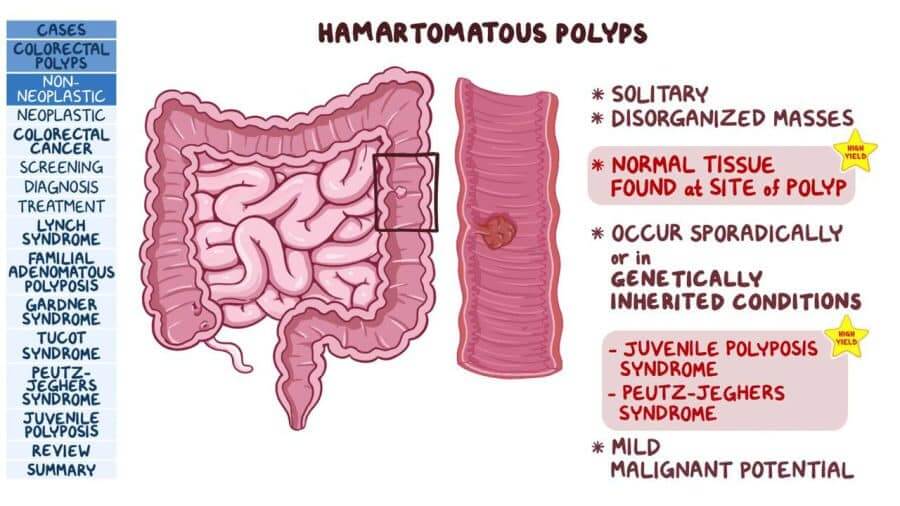
Guideline Topic: A summary of clinical features, current literature, and guidance for diagnosis, assessment, and management of patients with hamartomatous polyposis syndromes, with a focus on endoscopic management
Guideline development methods: A group of gastroenterologists reviewed recent data in PubMed between “2000-2018” in this area. Then synthesized both the data and the suggested approaches to diagnosis and management by other expert groups, and presented the consensus recommendations
Recommendations:
|
Questions |
Recommendations |
|
Peutz-Jeghers syndrome (PJS)
|
|
| Which individuals with hamartomatous polyps should be referred for genetic evaluation? | It is recommended patients with any of the following: undergo a genetic evaluation, have 2 or more lifetime hamartomatous polyps, have a family history of hamartomatous polyps, or cancer associated with a hamartomatous polyposis syndrome in first- or second-degree relatives. Genetic testing (if indicated) should be performed using a multigene panel test. (Strong recommendation, low quality of evidence) |
| Who should undergo a genetic evaluation for Peutz-Jeghers syndrome (PJS)? | It is recommended genetic evaluation for any individual with the following: 1) 2 or more histologically confirmed PJ polyps, 2) any number of PJ polyps in an individual who has a family history of PJS in a first-degree relative, 3) characteristic mucocutaneous pigmentation in a person with a family history of PJS, and 4) any number of PJ polyps in a person with the characteristic mucocutaneous pigmentation of PJS. (Strong recommendation, low quality of evidence) |
| Which organs should undergo surveillance when caring for a patient with PJS? | Patients with PJS are at increased risk for cancer in multiple organs, including cancer of the breast, small bowel, colon, stomach, pancreas, ovaries, testes, and lungs. Given this risk, It is recommended a multidisciplinary approach to cancer surveillance in these organs. (Strong recommendation, low quality of evidence) |
| How and when should small bowel surveillance be performed in PJS? | It is recommended that baseline small bowel surveillance using video capsule endoscopy or magnetic resonance enterography be performed between ages 8 and 10 years or earlier if the patient is symptomatic. If no polyps are found at the initial examination, surveillance should resume at age 18 years. Because of the risk of small bowel intussusception, small bowel surveillance in adulthood is recommended to continue throughout life every 2–3 years. (Strong recommendation, low quality of evidence) |
| What is the recommended approach to endoscopic surveillance of the stomach, duodenum, and colon in PJS? | It is suggested a baseline upper gastrointestinal endoscopy between the ages of 8 and 10 years, which could be performed at the time of capsule placement for small bowel surveillance or if polyps are identified on magnetic resonance enterography. Although the initiation age for colonoscopy remains uncertain, we also suggest initiation of colonoscopy at the same time as esophagogastroduodenoscopy. In those in whom characteristic polyps are detected, both colonoscopy and esophagogastroduodenoscopy should be repeated every 2–3 years. In those in whom there are no PJ polyps at baseline, surveillance is repeated at age 18 years, or sooner should symptoms arise, and then every 3 years. (Weak recommendation, very low quality of evidence) |
| What size polyps found on small bowel imaging in PJS should be removed? | It is recommended polypectomy of small bowel polyps that are symptomatic or ≥10 mm to prevent intussusception and other complications, such as bleeding. (Strong recommendation, low quality of evidence) |
| What is the recommended pancreatic cancer surveillance in PJS? | It is suggested annual pancreatic cancer surveillance with either magnetic resonance cholangiopancreatography or endoscopic ultrasound starting at age 35 years. (Weak recommendation, low quality of evidence) |
|
Juvenile Polyposis Syndrome (JPS)
|
|
| Who should undergo a genetic evaluation for JPS? | It is recommended genetic evaluation for any individual with 1) 5 or more juvenile polyps of the colon or rectum; 2) 2 or more juvenile polyps in other parts of the gastrointestinal tract; or 3) any number of juvenile polyps and 1 or more first-degree relatives with JPS. (Strong recommendation, low quality of evidence) |
| Which organs should undergo surveillance when caring for a patient with JPS? | Patients with juvenile polyposis syndrome are at increased risk for cancer in multiple organs, including cancer of the colon and stomach. Given this risk, it is recommended patients with JPS undergo surveillance of the colon and stomach. (Strong recommendation, low quality of evidence) |
| At what age should colonoscopic and upper endoscopic surveillance begin in individuals identified with JPS? | It is suggested to initiate colonoscopic and upper endoscopic surveillance at age 12–15 years, or earlier if symptomatic. Surveillance should be repeated every 1–3 years depending on the polyp burden. (Weak recommendation, low quality of evidence) |
| Which patients with JPS should undergo screening for hereditary hemorrhagic telangiectasia? | It is suggested patients with SMAD4 pathogenic variants be clinically evaluated for hereditary hemorrhagic telangiectasia at the time of the diagnosis, including screening for and appropriate management of cerebral and pulmonary arteriovenous malformations. (Weak recommendation, low quality of evidence) |
|
PTEN hamartoma tumor syndrome |
|
| Which gastrointestinal findings should prompt a genetic evaluation for PTEN hamartoma tumor syndrome? | It is recommended individuals with multiple gastrointestinal hamartomas or ganglioneuromas undergo genetic evaluation for Cowden’s syndrome and related conditions. (Strong recommendation, low quality of evidence) |
| Which organs should undergo surveillance for cancer when caring for a patient with PTEN hamartoma tumor syndrome? | In PTEN hamartoma tumor syndrome, patients are at increased risk for cancer in multiple organs, including cancer of the breast, thyroid, kidney, uterus, colon, and skin. Given this risk, it is recommended a multidisciplinary approach to cancer surveillance in these organs. (Strong recommendation, low-quality evidence) |
| What is the recommended colonoscopic surveillance in individuals identified with PTEN hamartoma tumor syndrome? | It is suggested colonoscopy surveillance to begin at age 35 years (or 10 years younger than age of any relative with colorectal cancer), repeated at intervals no greater than 5 years, depending on polyp burden. (Weak recommendation, low quality of evidence) |
|
Hereditary Mixed Polyposis Syndrome (HMPS) |
|
| There is not enough data to know the optimal surveillance intervals or whether extraintestinal neoplasia is a risk. The underlying genetic basis of the majority of HMPS families is unknown | |
Commentary:
| The treatment of JPS is concentrated on tumors that develop later in life when endoscopic methods are the basis of surveillance, as well as polyps that develop in childhood. To better understand the risk of cancer and the function of monitoring in the syndromes of PTEN hamartoma tumor syndrome, long-term prospective studies of mutant carriers are still required. Future research will use more robust cohorts of genetically described, less varied individuals as a result of advances in genetic testing and evaluation. Studying patients and families with unique phenotypes when no genotype can be identified is also necessary, though. Patients and families with uncommon phenotypes for which there is no genotype need to be studied |
Citation: C Richard Boland, Gregory E. Idos, Carol Durno, et all. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US multi-society task force on colorectal cancer. The American Journal of Gastroenterology. 2022; 117(6):846–864
DOI: 10.14309/ajg.0000000000001755
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
Topics: Hamartomatous Polyposis Syndromes, Colorectal Cancer